IVF can be performed using the intended mother’s eggs and/or the intended father’s sperm but if there is a medical concern with either partner, donor eggs or donor sperm is also an option. Also, in the case of same-sex male couples, donor eggs are needed for the IVF process. In the case of a same-sex female couple, donor sperm would be necessary.
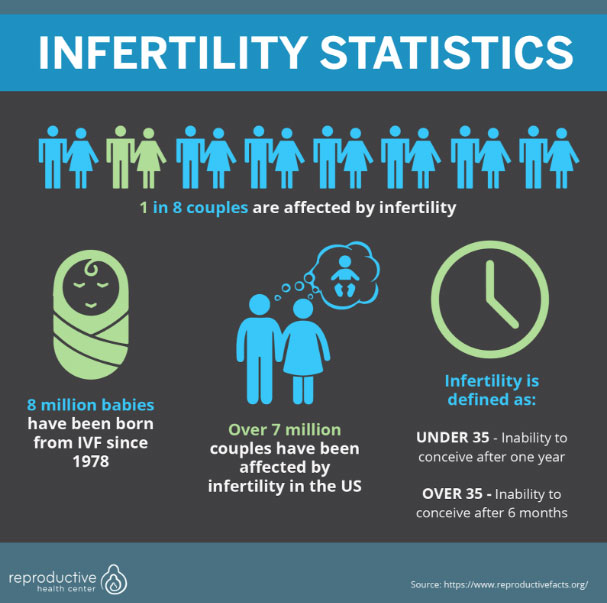
In the IVF process, eggs are retrieved and fertilized. Once an egg is fertilized, it is referred to as an embryo. The embryo will develop in the lab and will be either returned into the intended mother’s womb or a gestational surrogate with the ultimate goal of a healthy pregnancy and successful live birth. According to the most recent numbers in June of 2018, 8 million babies have been born through IVF since 1978.
Retrieval
The patient is under sedation during the egg retrieval process. The entire process takes no longer than 15 minutes. During the procedure, a fine needle is inserted through the vaginal wall and guided by ultrasound to remove the eggs from their follicle. After they are withdrawn from the ovary, the eggs will be taken to the lab for next steps.
The patient is then awakened from anesthesia and rests in our recovery room for approximately 20 minutes. It is recommended that the patient arranges for transportation and should be driving themselves home. Recovery is relatively painless. Some patients mention tiredness, bloating and mild cramping but this usually subsides within 24 hours. You may return to work the following day. Should you feel any pain or symptoms out of the ordinary, contact your doctor.
What Happens To My Eggs?
Several hours post egg retrieval, the eggs and sperm are brought together in-vitro (in the lab) or ICSI is performed. In cases where fertilization is with ICSI, sperm will be individually injected into the egg. The injected eggs will be monitored closely over the next couple of days to see if embryos are developing.
If the embryos have developed into a blastocyst (around day 5), the best are chosen for the transfer. If you and your doctor have discussed doing a fresh transfer, this will happen quickly. If you and your doctor have discussed a frozen transfer, this will happen according to a date that you have set prior to the procedure.
If you have chosen PGS or PGD testing, days 5 and 6 are the days when the biopsy will be performed. The lab will remove several cells from the embryo and send them to a separate genetics lab. The results will return in 10 – 14 days. Because of the wait, the embryos must be frozen. If you decide not to proceed with PGS or PGS, you can opt for a fresh transfer where the embryos are transferred back into the womb after the embryo has been in the lab for 5 – 6 days.
Transfer Process
The embryo transfer is the final step. Your physician performs this procedure. The physician will place the chosen embryo into a catheter and use ultrasound technology to guide the embryo, placing it into the uterus. Physicians take great pride in their embryo transfer techniques since this is such an essential part of the process. The procedure happens quickly and you do not need to be sedated. The patient can expect to go home within an hour after the procedure has finished.
The next 10 – 14 days can be nerve-wracking while you wait to take your pregnancy test. It is suggested not to take an at home pregnancy test during this time frame. The hormone that signals pregnancy (hCG) is also the same hormone that is in the trigger shot, so this could cause misleading results. Approximately 10 – 14 days post transfer, the patient schedules an appointment for a blood test to determine early pregnancy results.

Fertility Medications
After the birth control stops, you will be directed to begin taking injectable fertility medications. Prepare to be on fertility medications for 10 – 12 days. The number of days could be slightly less or more depending on hormone levels and follicle sizes.
Throughout the next 10 – 12 days you will self-administer multiple daily injections and visit the clinic for blood work/monitoring several times. Monitoring appointments are in the morning so clinics can provide the results by afternoon. Once we review your results, a provider from your clinic will call you to provide updates and next steps. Towards the end of the 10 to 12 day window, the frequency of monitoring visits will increase. This is because the clinic needs to carefully watch your follicle sizes and hormone levels so that your trigger shot can be scheduled at the perfect time.
Once you’ve reached a point during stimulation where your follicles are an ideal size, you will be instructed to take the trigger shot. This is a separate fertility medication that will trigger ovulation. 36 hours later, your egg retrieval will be scheduled. Timing is crucial during this segment of the IVF procedure.
Egg Retrieval
During the egg retrieval procedure, sedation will be administered by an anesthesiologist. Once you are sedated, a fine needle is inserted through the vaginal wall and guided by ultrasound towards the follicles. The eggs are then removed from their follicle and withdrawn from the ovary. The entire egg retrieval process will take approximately one hour which includes sedation, the procedure, and recovery. Meanwhile, the eggs are whisked away to the lab.
After the eggs spend just a few hours in the lab, they are placed with the sperm in a dish or injected with sperm through ICSI. At RHC, we suggest ICSI to increase the chances of successful fertilization. The following day, the embryologist will provide a report detailing how many eggs fertilized. Then, the embryo culture process begins.
Embryo Development
Over the next few days, embryologists will closely monitor the development of eggs and sperm until ideally, they reach the blastocyst stage. The blastocyst stage occurs when the embryo has developed both an inner and outer cell mass. This usually happens after 5 – 6 days in the lab. At RHC, we will provide patients with a report stating the number of blastocysts that have developed.
It is important to note that it’s normal for attrition to happen. There will be a significant difference between the number of eggs and the number of blastocysts created. For example, if 15 eggs are retrieved, it is common to expect 2 – 4 blastocysts. Some eggs are not normal at retrieval, some eggs just won’t fertilize for unknown reasons, some embryos arrest their development during the culture process and some blastocysts will be genetically abnormal.
If you have chosen to have PGS or PGD, the embryos will be biopsied as they reach the expanded blastocyst stage. This is done by making a microscopic hole in the embryo with a fine-tuned laser. The embryologist can then can tease out a few cells to be sent to the genetic testing company for DNA analysis. Expect results within 10 days. The embryos are then frozen to await transfer. You can expect your period to start between 5 – 10 days after the egg retrieval. If you choose not to do PGS or PGD and prefer a fresh transfer, the selected embryo/s will be placed back into the patient on transfer day.
Uterine Lining Receptivity Testing
At this point, all of the embryos have been made. For some patients, there is a step between making the embryos and embryo transfer. If you have experienced any of the following in previous cycles, an endometrial receptivity assay (ERA) may be a good option for you.
- Pregnancy Loss
- Implantation Failure
- Less than 3 normal embryos post PGS or PGD
- A diagnosis of the luteal phase defect
- 37 or older
What is an endometrial receptivity assay (ERA)?
An ERA test determines the optimal time for embryo implantation. If an ERA is determined as the best next step, you will be put on the protocol for embryo transfer (see step 5). Instead of performing a transfer though, the clinic will take a biopsy of your uterine lining. The sample of the uterine lining is sent to a company that specializes in ERA testing (RHC uses Igenomix). This test will identify the window of implantation and then recommend the best time for an embryo transfer. By transferring during your uterine linings best window, the chances of a successful outcome are increased.
Embryo Transfer
Here are a few things you need to know about the embryo transfer process:
- If you and your doctor have decided on a fresh transfer, this process will begin 5 – 7 days after your retrieval. If you and your doctor have decided on a frozen transfer, it would be scheduled according to a predetermined date.
- At RHC, 90% our patients opt to have a frozen embryo transfer not only because it allows your body to recover from the egg retrieval process, but it will enable for PGD, PGS, and endometrial receptivity testing which all enhance the chances of a successful pregnancy.
During the next few points, we will discuss a process that is a bit more specific to our RHC protocol. Please keep in mind your individual clinic’s protocols may vary slightly.
- To prepare the uterus, RHC typically prescribes estradiol tablets. About six days before transfer, the patient will begin progesterone medication. A spreadsheet or tracker is usually provided to keep all appointments and medications organized.
- Find someone that can drive you to and from the appointment or arrange transportation. This is imperative because you will be prescribed a muscle relaxer prior to transfer, and will not be able to operate a vehicle.
- Your physician will perform the embryo transfer procedure. The chosen embryo is placed into a transfer catheter, and ultrasound technology is used to guide the embryo, placing it into the uterus.
- After transfer, you will be given instructions to take it easy for several days. It’s important to keep in mind that nothing you do at this point can affect implantation success. It is also best not to administer a self-pregnancy test at home.
- A pregnancy test is taken 10 – 14 days after transfer either in our clinic or at a lab that your insurance approves.
- If you are pregnant, you will continue your current medication protocol through about 12 weeks of gestation.
- A pregnancy ultrasound is done at the 6 to the 7-week mark.
- At the 12-week mark, you’ve graduated from your Reproductive Endocrinologist! You are now at a point where your pregnancy is healthy, and you can begin seeing your OB/GYN for the duration of gestation.
If you are not pregnant, you will speak with your provider and decide together on next best course of treatment. RHC is here to guide you and provide support every step of the way.
Since there are multiple steps to the IVF process, you will likely interact with multiple providers during the process. Each clinic has slightly different protocols and views on which providers should be involved at which step.
At RHC, we pride ourselves on the fact that our physicians are involved in every step of the process. Our physicians perform each ultrasound, call back each patient with the results, and perform both the retrieval and transfer. In addition, board certified anesthesiologists administer anesthesia during your egg retrieval and transfer procedures. It is a standard practice that physicians perform both egg retrievals and transfers, but larger clinics often have ultrasound technicians perform ultrasounds and nurses doing the callbacks. In addition, large practices can also rotate physicians depending who is on call and therefore, you can get a different physician during your egg retrieval and/or transfer. Be sure to ask these questions up front so you are aware of the provider’s involvement in your IVF journey.
Before determining if IVF is the best option for you, it’s important to have a consultation with a Reproductive Endocrinologist to discuss your individual situation and history. IVF is not for everyone and these are some of the patient types in which IVF is not recommended:
- When a simpler procedure (for example – intrauterine insemination or IUI) can help you achieve pregnancy, a procedure like IVF is not recommended.
- IVF is not recommended for those that can conceive naturally.
- IVF is not recommended for women over the age of 44 using their own eggs. This is because the chance of success is low but the chance of genetic abnormalities and miscarriage is high. If you’d like to have a child over the age of 44, it is recommended to use donor egg option.
- IVF is not recommended for women over the age of 50, even with donor eggs. This is due to the concern for the safety and health of the woman giving birth over the age of 50.
- IVF is not recommended for people with a BMI of over 35 or under 18.
- A patient has a greater risk of complications if their BMI is above 35. However, it’s important to note that even just a 10% reduction in body weight can result in a significant difference in the safety and health of the patient, in addition to the chances of success. The same rings true for patients that have a severely low BMI. If you’re BMI is too low, it can affect ovulation and your menstrual cycle. Although this is not true for everyone, it is recommended to have a BMI within a healthy range before undergoing IVF.
These are general guidelines, but it’s important to discuss your case with your provider and clinic to determine if IVF is right for you.
The best way to select a gender with IVF is through PGS testing. All eggs begin as females until the sperm brings the X or Y chromosome to match. This determines the gender. PGS is very effective at determining the gender of the embryo. As we discussed above, by removing a small number of cells from the embryo on day 5, we can test those cells for the X or Y chromosome. Then, once we know which embryos are male or female, the couple can decide which embryo to implant. If additional embryos are remaining, they will be frozen for later use.
Now that the embryo has been transferred, you will likely feel relieved, elated but also nervous. This is normal. It’s important to surround yourself with a good support system and remember, there is nothing you can do to increase the chance of success at this point. Keep stress to a minimum and engage in light activities once again. You will continue your progesterone medication throughout the next 10 – 14 days. Progesterone is a hormone that thickens and maintains a strong uterine lining which is crucial for successful implantation.
In the 10 days from transfer to the pregnancy test, a lot of miraculous things are happening inside the body.
During day 1 and 2 post transfer, the embryo is just beginning its hatching stage and begins to attach itself to the uterine lining.
Throughout the next few days, the embryo will further attach itself. You may experience a tiny bit of bleeding during this stage although it varies from person to person.
As the embryo attaches further it begins developing cells that will eventually become the placenta. This is what secretes HCG. This hormone triggers the body to release more progesterone which strengthens the uterine lining and future fetus. By day 10, the HCG should be detectable in the bloodstream.
You will be scheduled for a pregnancy test in a clinic or lab 10 – 14 days post transfer. If hCG is detected through a blood test, this will signal that there is a successful implantation. If a pregnancy is detected, the clinic will monitor you closely until the 6 – 7-week mark when an ultrasound is performed. When the 12-week mark is reached, the Reproductive Endocrinologist will kindly say goodbye as our job is done. You will then see your OB/GYN for the duration of your pregnancy.
If a pregnancy is not achieved, your provider will discuss with you the best next steps. Rest assured many couples that do not achieve pregnancy during the first round of IVF go on to have multiple successful pregnancies on subsequent rounds. The most important thing is to maintain hope and trust that an optimal course of treatment will be next.
ICSI stands for intracytoplasmic sperm injection. ICSI is a procedure that aids the sperm in fertilizing the egg. With conventional IVF, the egg and sperm are placed in a dish and the sperm fertilizes the egg “naturally”. ICSI is slightly different because it provides the sperm with some assistance. During the ICSI procedure, an embryologist chooses one sperm and places it on a fine needle. It is then injected directly into the egg.

The embryologists will be sure to choose the best quality sperm before injecting. By providing the sperm with a bit of assistance, it is substantially increasing the chances of fertilization.

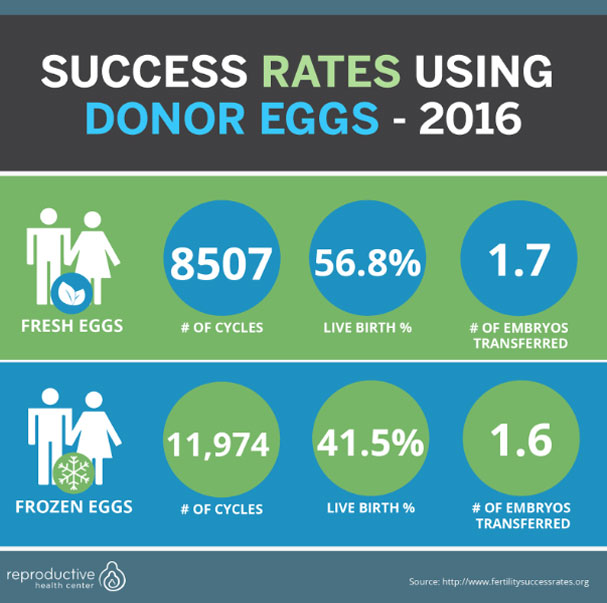
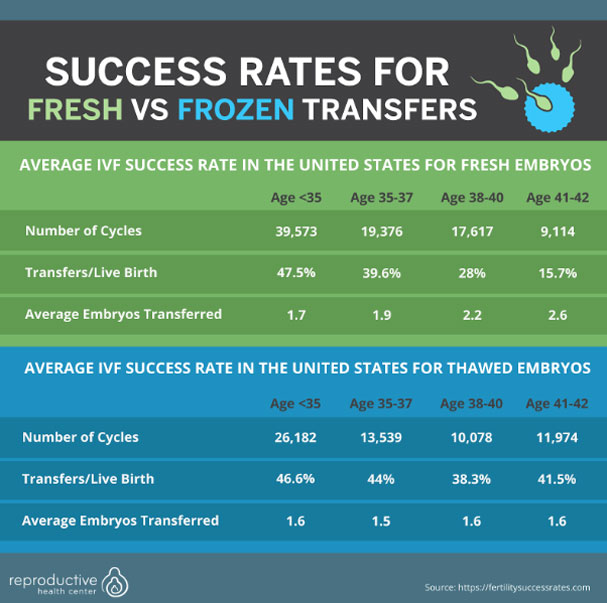
We have provided an average below based on the 2016 success rates from fertilitysuccessrates.com which is generated based on data from the CDC (center for disease control). Your individual clinic should also be able to provide their success rates. Please note, these are often a year or two behind because of the time it takes patients to go through fertility treatment and become pregnant.
| Age | Fresh | Frozen |
| Under 35 | 47.5% | 46.6% |
| 35 – 37 | 39.6% | 44.0% |
| 38 – 40 | 28% | 38.3% |
| 41 – 42 | 15.7% | 32.1% |
| Egg Donation | 56.8% | 41.5% |
It’s important to note that not every clinic within the United States is included in this report, however, this does provide a very reliable look at the nationwide average.
It’s also important to note that even without IVF, a healthy woman under the age of 35 only has a 25 – 30% chance of getting pregnant every month and after 35 it declines further. A woman between the ages of 36 – 40 has a 10 – 15% chance and that number drops to below 5% over the age of 40.
The best way to get started with IVF is to speak to a Reproductive Endocrinologist to understand if IVF is the best course of treatment. Sometimes, the need for IVF is obvious if you have conditions like endometriosis or low sperm count requiring intervention. However, for approximately 30% of couples who have unexplained fertility, it might not be so obvious. Luckily, there are suggested parameters so you know when it’s time to seek fertility assistance.
A woman under 35 who has not conceived after 12 months with unprotected and contraceptive-free intercourse
A woman over 35 who has not conceived after 6 months of unprotected or contraceptive-free intercourse
If you are in a same sex male relationship and would like to have a child through the assistance of donor eggs and a gestational surrogate or if you’re in a same sex female relationship and would like to have a child through Reciprocal IVF
If you have spoken to your OB/GYN about your fertility, ask for a referral or guidance to a Reproductive Endocrinologist. Although OB/GYN physicians are excellent doctors, their specialty lies in caring for a woman’s day to day health and a pregnancy once it’s been achieved. The process of getting pregnant can be quite detailed and requires a specialist such as a Reproductive Endocrinologist.
Once you have chosen your clinic/provider, the first step is to schedule an initial consultation for blood work and exams. By learning more about your current state, your specialist can address the best next steps. In some cases, IVF is not needed and other more simple approaches may be taken. However, it’s impossible to determine the next steps without an initial fertility consultation. Once the results are in, a provider will talk to you about the best next course of treatment.
The medications you take during treatment will depend on your situation. Here are the most common medications prescribed during IVF.
An agonist or antagonist
You will likely be prescribed either an agonist or an antagonist during your stimulation. These medications suppress your hormones so natural hormones do not interfere with prescribed hormones. It has not been determined that one is more successful than the other. With an agonist like Lupron, you will start injections a few weeks before you start your hormones. This is because, upon initial injection, Lupron will increase the amount of estrogen in your body. Then, over the following days, it gradually decreases. The opposite is true with an antagonist. An antagonist reacts immediately and is a blocker that works on your pituitary gland, so all of your hormones are immediately suppressed. Therefore, you will likely start an antagonist (Ganirelix or Cetrorelix/Cetrotide) around day 4 – 6 of stimulation. Antagonists require a significantly less number of injections. However, depending on your case and history your provider may prefer one protocol over another.
Gonadotropins
Gonadotropins are hormones that mimic FSH and LH that naturally occur in your body. You will likely be prescribed an FSH (Follistim or Gonal-F) and/or an HMG (Menopur). HMG is a combination of FSH and HCG driven LH activity. Different clinics and providers have different preferences on which dosages and medications to use. It’s also likely your dosages will be adjusted throughout your stimulation based on your follicle size and estrogen levels.
HCG
HCG is used in two different ways during fertility. This hormone is produced in the body to signal pregnancy. But, because HCG is similar structurally to LH, some physicians use it during stimulation. In addition, HCG is also used to trigger a patient during the end of stimulation to induce ovulation and complete the egg maturation process.
Progesterone
Progesterone has many roles and is crucial to the IVF process. Progesterone medications thicken a woman’s lining so the embryo can properly attach. If pregnancy occurs, the placenta eventually creates progesterone to sustain the lining and aids in developing the fetus. Progesterone can be taken through progesterone in oil injections or vaginally through approved vaginal gels or suppositories (Crinone or Endometrin). A patient will normally be prescribed progesterone for 10 – 12 weeks until the placenta can produce progesterone independently.
The following medications should be refrigerated. Medications not listed should be stored at a room temperature of 59 – 86 degrees Fahrenheit.
- Cetrotide (antagonist)
- HCG (store refrigerated after mixed/reconstituted)
- Leuprolide Trigger Shot
- Microdose Lupron
- Novarel (only needs to be refrigerated after reconstitution)
- Ovidrel
- Gonal F pens
- Follistim Cartridges
If you doubt whether or not to refrigerate, err on the side of caution and refrigerate the medication. You can also consult the drug’s package insert (the white brochure that comes folded in all of the medication packages) if you’d like the specifications for storage.
Medications are an essential part of the IVF process but they do come with some side-effects. Before we start, it’s important to note that no credible studies have linked an increased risk of cancer with fertility medications. Even one Cochrane Review (one of the most dependable sources for unbiased medical research) looked at 13 years of data, from 25 studies and over 182,000 women. It concluded there was no correlation between fertility medications and ovarian cancer.
“We found no convincing evidence of an increase in the risk of invasive ovarian tumors with fertility drug treatment.” – Cochran
Review
Here are some of the most popular medications used during stimulation and their associated side effects.
Clomiphene Citrate (CC or Clomid)
Clomid is used to induce ovulation in women that do not develop and release an egg (ovulate) on their own. Clomid is also used to stimulate extra follicles and eggs in the ovaries of women that already ovulate without medications. In Clomid’s initial approval trial the following side effects were noted:
Ovarian Enlargement (this is natural as your ovaries are indeed getting larger as the follicles grow)
- Hot Flashes
- Abdominal Discomfort/Bloating
- Nausea
- Vomiting
- Breast Discomfort
- Blurred vision and Headache
- Spotting
Letrozole (Femara)
Letrozole is used in fertility treatment when a woman has problems ovulating. Although it is also widely used as a breast cancer treatment, it can also work in fertility patients because it induces ovulation. The most common side effects include:
- Hot Flashes
- Hair loss
- Nausea
- Diarrhea
- Drowsiness
- Headaches
- Constipation
Follicle Stimulating Hormone (FSH)
You may recognize your FSH medications by the names Gonal-F or Follistim. These medications are injectables that are delivered through cartridges and pens. Common side effects include:
- OHSS (ovarian hyperstimulation syndrome)
- OHSS happens when the ovaries become swollen with fluid. Severe OHSS happens in less than 1% of patients, but it can be serious when it happens. If you feel you are in danger of this during your cycle, contact your provider or ER immediately.
- Bloating
- Abdominal Pain
- Mood swings
- Injection Site reactions such as redness, itching, and swelling
Human Menopausal Gonadotropin (HMG)
You may recognize this medication by its more common name Menopur. Menopur comes in a small vial and is injected subcutaneously. It also has the following side effects:
- OHSS (ovarian hyperstimulation syndrome)
- OHSS happens when the ovaries become swollen with fluid. Severe OHSS happens in less than 1% of patients, but it can be serious when it happens. If you feel you are in danger of this during your cycle, contact your provider or ER immediately.
- Headaches
- Abdominal Pain and Bloating
- Breast enlargement and tenderness
- Nausea and vomiting
- Injection site redness
- A slight burning sensation at the injection site
Agonist (Lupron)
Lupron (or Leuprolide) is used to reduce your estrogen and indicated for patients with endometriosis. Upon first administration, agonists cause a surge in hormones but then slowly shut them down after a few days. They are usually started before IVF treatment begins. Because Lupron reduces estrogen, many symptoms mirror that of menopause. These include:
- Hot flashes
- Headache
- Decreased sex drive
- Mood swings
- Vaginal dryness
- Nausea
- Weight gain
- Decreased sex drive
- Dizziness
- Injection site soreness
Lupron can also be used to trigger ovulation. It is often preferred by physicians to trigger ovulation in patients that have high follicle numbers or high estrogen levels during the IVF cycle.
Antagonist (Ganirelix or Cetrorelix/Cetrotide)
Unlike an agonist or Lupron, antagonists like Ganirelix or Cetrotide do not cause an initial surge in hormones. Instead, they work by blocking and suppressing hormones immediately. Therefore, the number of injections and length of time taking injections is shorter which equals fewer side effects.
However, some side effects are still present and these include:
- Abdominal pain and tenderness
- Headache
- Nausea
- Injection site soreness
- Abnormal menstrual bleeding/spotting
Trigger Shot – HCG (Novarel, Pregnyl, Ovidrel, Lupron 4 mg)
When it’s time to trigger the patient and induce ovulation, you will likely be told to take Lupron or HCG or both. This will only happen once during your stimulation, as the trigger shot will cause the eggs to complete their maturation getting them ready for retrieval. You will be asked to inject the trigger shot(s) at a very specific time.
Common side effects include:
- Vomiting
- Nausea
- Abdominal Pain/Swelling
- Headache
- Weight gain
- Breast tenderness
- Redness/pain/bruising at the injection site
Progesterone
Progesterone is used to supplement a pregnancy and thicken the uterine lining so the embryo has the best chance of a successful implantation. There are several ways in which progesterone can be administered.
- PIO (progesterone in oil) – these injections are taken intramuscularly
- Vaginally with capsules (Prometrium)
- Progesterone suppositories made by a pharmacy
- Vaginal Gel (Crinone) or Vaginal Suppositories (Endometrin)
Side effects will vary slightly based on if the medication you are prescribed is administered by injection or vaginally. For example, PIO injections can result in injection site reactions and the medications administered vaginally have a higher chance of a discharge. However, progesterone will usually have the following side effects:
- Headache
- Breast tenderness
- Drowsiness
- Dizziness
- Bloating
- Hot flashes
- Abdominal pain
It is important to note that every patient will experience slightly different side effects. Your body is going through a lot, so try to relax and reduce stress. If you have specific questions about side effects regarding your medication, talk to your provider.
Performing IVF without medication is possible. Some patients investigate this option because it eliminates the risk of OHSS and reduces the use of hormones resulting in a lower medication cost.
However, RHC discourages the use of IVF without fertility medication. This is because IVF is a process that can take weeks to months. And, depending on how many cycles you undergo, it can become quite costly. Therefore, in order to maximize your chances of success while undergoing the least amount of treatment possible, it makes the most sense to use fertility medications. Medications will cause your body to grow multiple eggs, which is a good thing because you will need multiple eggs to make multiple embryos. If you choose not to use medications during IVF, your body will only grow one egg at a time. If the one egg does not become an embryo than you must start the process from the beginning. The most expensive part of the IVF cycle takes place in the laboratory. The cost for lab services is the same with one egg or 20. So, to optimize your chances of success, we recommend fertility drugs during the IVF process. We encourage you to speak with your provider and clinic further if you are interested in an IVF cycle without medication.
The acronym PGS stands for preimplantation genetic screening. PGS is a test that will determine if an embryo is genetically normal. A healthy embryo has 46 chromosomes and 23 pairs. A chromosomally normal embryo is referred to as euploid. If the embryo does not have 46 chromosomes, it is referred to as aneuploidy. It is commonly thought that the main reason IVF fails is that the embryo implanted is genetically abnormal or does not have all 46 chromosomes.
PGS is performed once an embryo reaches the blastocyst stage (around day 5 post retrieval). The embryo is biopsied by making a microscopic hole in the embryo with a fine-tuned laser. The embryologist then can tease out a few cells to be sent to a genetic testing company for DNA analysis. Results typically return within 10 days.
At RHC, we suggest PGS for all of our patients as it increases the chance of success and reduces the chances of having a child with a genetic abnormality. An abnormal number of chromosomes is thought to be the main reason why women have miscarriages and difficulty conceiving in their late 30s and early 40s. Even in a natural pregnancy, if an embryo has an abnormal number of chromosomes, it is less likely to implant and results in a pregnancy.
The ultimate goal of PGS testing is to identify and transfer the healthiest embryo, ensuring the highest chance of a successful live birth. However, because just a few cells are representing the entire embryo (a day 5 embryo has approximately 200 cells), it is important to note that PGS is not a guarantee.
PGD is an acronym for preimplantation genetic diagnosis. While PGS tests for the correct number of chromosomes, PGD tests for a specific genetic defect. The process for PGS and PGD are the same. Once the embryo has reached blastocyst stage (day 5 post retrieval), it is biopsied, and several cells are sent to a genetic lab for testing. PGD can be used to test for over 400 genetic conditions. Some of the most common genetic conditions include:
- Cystic Fibrosis
- Huntington’s Disease
- Tay Sachs
- Muscular Dystrophy
- Sickle Cell Anemia
If you want to test for a specific disease, even if you have no fertility issues, you will still need to undergo the process of IVF. Some couples know that a specific genetic issue runs in their family and/or they happen to be a carrier for a disease they do not want to be passed down to their offspring. Once the test is returned in 10 days, couples can decide which embryos to transfer.
The success of IVF treatment depends on several different factors. Every patient’s situation is unique. While in some cases it is very easy to determine why IVF was unsuccessful, sometimes there are unexplained reasons as to why IVF didn’t work. Here are the most common factors that lead to an unsuccessful IVF cycle.
Poor egg quality
Egg quality is one of the major indicators of a successful IVF treatment. If egg quality suffers because of things like age or lifestyle factors, it will be very difficult to make a good embryo that will result in a pregnancy.
Poor ovarian response
Not every patient responds to fertility medications in the same way. If stimulation does not yield a solid number of eggs, it will be tough to make a good embryo. However, it’s important to remember that you only need one good egg. So even if you have a low ovarian reserve, it’s very possible you can still retrieve enough eggs to make an embryo.
Lifestyle
Lifestyle factors impact your egg quality. Factors like smoking, poor diet and a BMI that is too high or too low can impact fertility.
Poor quality uterine lining (endometrium)
If your uterine lining is not optimal, it can be very difficult for an embryo to implant. The uterine lining, also called the endometrium is the place the embryo implants, and if the lining is not receptive or of poor quality (too thin, too thick or if uterine polyps or adhesions are present) establishing a good pregnancy is difficult. If recurrent miscarriages or repeated implantation failure occur, an Endometrial Receptivity test may be performed to determine the best day for implantation. At RHC, we are supporters of this test because we’ve seen it increase the chances of successful pregnancies in our patients.
Genetic Abnormality
In a natural pregnancy, some embryos that have genetic abnormalities will fail to implant. However, we often don’t know this is occurring because it happens early and patients get their periods as normal. However, it is much more evident in IVF treatment because of how much we are investing and monitoring every step of the process. By performing PGS or PGD tests on embryos, we can better determine the healthiest embryos and therefore only transfer those. While this is not a 100% guarantee, it does greatly increase the likelihood of a healthy pregnancy. RHC is a firm supporter of these genetic tests because of the positive results we’ve seen in our patients.
Unexplained
Unfortunately, we do not always know why IVF was not successful. Based on years of experience and the latest technology, providers can often narrow down the potential issue and suggest the best next step.
There are several differences between fresh and frozen transfers. A fresh transfer used to be commonplace and yield better results. However, recent research and technology have shown us that freezing the embryos after the stimulation cycle to produce eggs improves the pregnancy rates. We will discuss the two options below.
Fresh Cycles
In a fresh cycle, a woman undergoes stimulation as normal, with the goal of retrieving as many eggs as possible. The eggs become embryos in the lab by either being injected with sperm (through ICSI) or left to fertilize by their own devices. This process takes 4 – 6 days. If you have a fresh transfer, you are preparing your body for the transfer of these embryos at the end of those 4 – 6 days. This is a quick turnaround and for some women, can be a little stressful. With a fresh transfer, the best embryos are chosen by a visual grading test. Therefore, we cannot determine, with certainty, which embryos have genetic deficiencies. With frozen transfers, we can perform tests that help us determine which embryos have genetic abnormalities. If any embryos remain, they will be frozen for future use. We typically perform fresh transfers to women who are receiving donated eggs or embryos.
Frozen Cycles
In order to initially retrieve eggs, every woman must go through hormone treatment. However, when you elect a frozen transfer, you will have gone through hormone treatment weeks or months prior, so your body will have time to rest. Patients will have to be on some medications prior to embryo transfer (likely progesterone and/or estrogen) but it’s not nearly as invasive or intense as hormone injections. These medications will prepare your lining for embryo implantation.
Frozen cycles can also be scheduled months or weeks in advance, allowing for more control over the timing of the cycle. Frozen transfers are beneficial because they give providers the ability to do tests like PGS, PGD and Endometrial Receptivity testing that have been shown to increase the chances of successful pregnancies and reduce genetic abnormalities. This can only be done when electing to have a frozen transfer cycle because of the time it takes to receive the results.
Several patient types may need IVF. These include:
- Patients who have attempted to conceive for over one year with no successful pregnancy (if under 35) or patients that have attempted to conceive for six months with no successful pregnancy (if over 35).
- A patient who is a carrier of a genetic disorder that does not wish to pass it on to their offspring.
- Patients that would like to use frozen embryos, donor eggs, donor sperm or donor embryos.
- A patient with a history of recurrent miscarriages.
- Same-sex couples.
- Unexplained infertility.
- Physical impairments that prevent natural conception.
- Tubal Ligation.
- Vasectomy.
- Endometriosis.
If you’re questioning if IVF is right for you, RHC has providers on staff who are happy to discuss your individual situation.
Determining if you are a good candidate for IVF depends on your individual situation. Here are some general guidelines for determining your candidacy:
- If you are under 35 and have been trying for one year without contraception.
- If you are over 35 and have been trying for 6 months without contraception.
- If you have not been successful with less invasive procedures, such as intrauterine insemination (IUI) or Clomid cycles, it may be best to move forward with IVF instead.
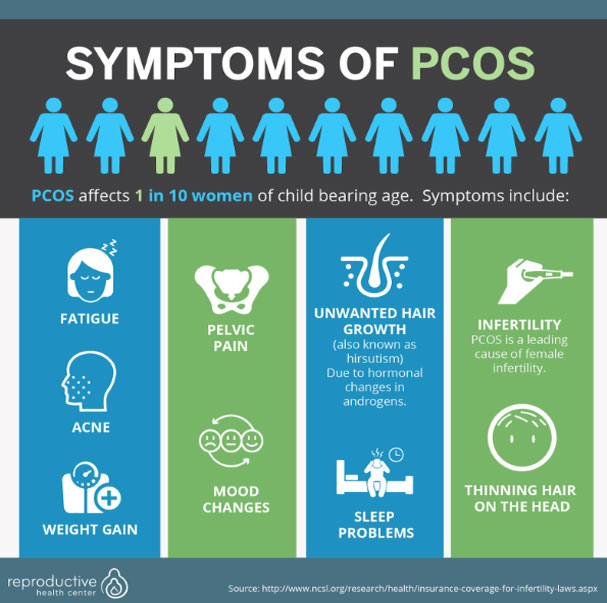
- Polycystic Ovarian Syndrome (PCOS) is a hormonal disorder in which the ovaries can develop small bits of fluid (follicles) and do not release eggs. PCOS patients generally have more difficulty conceiving because they do not ovulate and therefore, are good candidates for IVF.
- Endometriosis is an extremely painful disorder where the endometrium grows outside of the uterus. This can affect the function of the ovaries and the fallopian tubes, limiting the chance of pregnancy.Patients with endometriosis who have been having trouble conceiving are good candidates for IVF.
- If you have any blockage, scarring or damage to your fallopian tubes it will be very difficult to get pregnant naturally. Therefore, IVF is a great option because it circumvents the fallopian tubes.
- If a patient has male factor infertility, low sperm count or poor quality sperm, IVF and ICSI can circumvent the problem. ICSI is a procedure that takes the best sperm and injects them directly into the egg greatly increasing the chances of success. Patients with male factor infertility issues are great candidates for IVF because the only way to perform ICSI is to undergo the IVF process.
- Same-sex couples that use donor egg or sperm will require IVF.
- Patients who are at risk or carriers for genetic diseases and do not want the disorder passed to their offspring are good candidates for IVF.
It’s best to talk to your provider and set up an appointment with a Reproductive Endocrinologist to determine your candidacy for IVF.
Once IVF treatment has been chosen as the best course of treatment for your individual case, IVF will be scheduled several weeks to several months in advance. Different physicians and clinics have different waiting times, and it’s important to you pick a time where you can be home and have limited stress for an extended period of time.
Both IVF egg retrievals and transfers are done within or next to the clinic’s lab. This is because the eggs retrieved are taken directly into the lab before or after the procedures. Also, the same is true when the embryos are transferred to the patient. Some clinics have their lab at the same location as their office, and other clinics have them off site at a hospital or outpatient facility. Regardless of the location, the procedure is always outpatient, and the patient can return home on the same day.
Speak with your clinic to ensure you know the location and address of the lab and where the procedures will be held. At RHC, our lab is at the same location as our clinic making it much easier for our patients. Because these procedures are scheduled early in the morning, you will want to make sure transportation is scheduled ahead of time.
It is very possible IVF will work the first time, however, each case is unique so you must first speak with a Reproductive Endocrinologist to determine your chances of success. IVF success rates are available online at the website for the Center for Disease Control (CDC) and the Society for Assisted Reproductive Technology (SART). On these websites, you can see the average rates for the entire country, individual states, and clinics.
At RHC, we take a unique and direct approach to increase the chances of a successful first IVF cycle. For example, RHC performs PGS (preimplantation genetic screening) on nearly every embryo. PGS determines which embryos have the correct number of chromosomes. If your embryo does not have 46 chromosomes, this can cause genetic defects, resulting in miscarriage or failed implantation. Therefore, by determining the healthiest embryos before your first IVF cycle, you will increase the chances of IVF working the first time.
When choosing a provider, ask what tests can be done during the first cycle to ensure the ultimate chance of success the first time. In addition, make sure you reduce smoking and make healthy lifestyle choices to increase your chances of an optimal IVF cycle.
Speak with your clinic to ensure you know the location and address of the lab and where the procedures will be held. At RHC, our lab is at the same location as our clinic making it much easier for our patients. Because these procedures are scheduled early in the morning, you will want to make sure transportation is scheduled ahead of time.
IVF itself is not painful. While you are undergoing both the egg retrieval and transfer procedure, you will be under twilight or light anesthetic. So although you will not feel pain during the procedure itself, you may feel pain or slight discomfort before or after the following:
During stimulation, you will self-administer hormone injections. Some patients experience slight burning and tingling at the injection site. Also, the side effects of the hormones can result in headaches, fatigue, and bloating especially towards the end of stimulation as your ovaries are enlarged.
You may feel slight abdominal pain and bloating after your egg retrieval and transfer. Remember, your body is undergoing a lot of things at once, and your hormones are fluctuating. Be patient and be sure to get some rest.
There’s no doubt that any pain associated with IVF is not just physical, but can cause mental stress as well. At RHC, we can guide you towards a psychologist if you feel like you need someone to speak with. In addition, we encourage activities like acupuncture and yoga that aid in stress relief and compliment IVF.
If any of your symptoms become severe, such as extreme weight gain, nausea or vomiting, it’s possible you could be at risk for OHSS (ovarian hyperstimulation syndrome). Contact your provider immediately if you feel any of these symptoms during stimulation or after your procedures.
At RHC, we take a unique and direct approach to increase the chances of a successful first IVF cycle. For example, RHC performs PGS (preimplantation genetic screening) on nearly every embryo. PGS determines which embryos have the correct number of chromosomes. If your embryo does not have 46 chromosomes, this can cause genetic defects, resulting in miscarriage or failed implantation. Therefore, by determining the healthiest embryos before your first IVF cycle, you will increase the chances of IVF working the first time.
When choosing a provider, ask what tests can be done during the first cycle to ensure the ultimate chance of success the first time. In addition, make sure you reduce smoking and make healthy lifestyle choices to increase your chances of an optimal IVF cycle.
Speak with your clinic to ensure you know the location and address of the lab and where the procedures will be held. At RHC, our lab is at the same location as our clinic making it much easier for our patients. Because these procedures are scheduled early in the morning, you will want to make sure transportation is scheduled ahead of time.
Endometriosis is a painful condition that affects nearly 5 million women in the United States. The lining of the uterus is called the endometrium. If you have endometriosis, this lining grows in places outside of the uterus. It can also leave scarring, create cysts on the ovaries, and or lesions or blockages in your fallopian tubes which all impact fertility. In addition, this condition can be extremely painful. The good news? Pregnancy is still possible with endometriosis and IVF is a tremendous option.
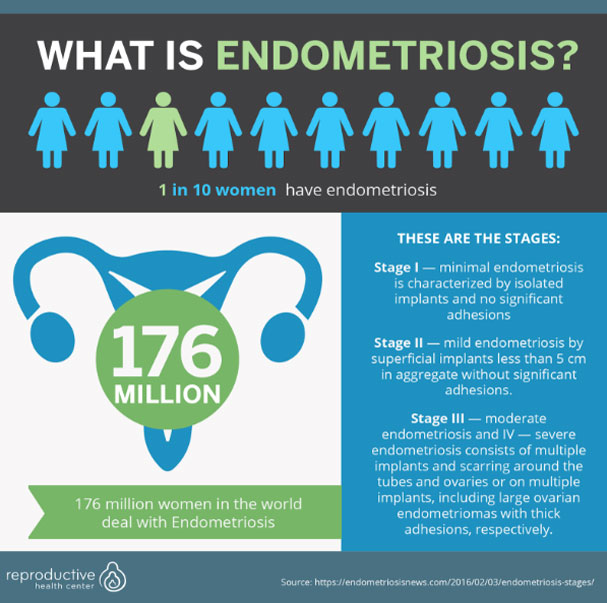
The first step is to schedule a consultation with a Reproductive Endocrinologist to help diagnose if, in fact, the patient does have endometriosis and then determine the impact on the patient’s fertility. Once the provider has determined the cause, surgery or medications may be an option. At RHC, we have had many patients diagnosed with endometriosis that have gone on to have healthy and successful pregnancies.
PCOS is an acronym for polycystic ovarian syndrome. In PCOS, women do not ovulate normally or ovulate at all, making it difficult to conceive. Women with PCOS tend to produce a high number of eggs when given fertility medications and have an increased risk of multiple gestations (twins or greater) with ovulation induction (with insemination or intercourse). Their risk of multiple gestations is reduced with IVF because only one embryo is transferred. Additionally, PCOS patients may produce in excess of 20 eggs during an IVF cycle. Some of these eggs will not be at a stage that allows them to be fertilized (these are considered premature oocytes and post mature oocytes). During the embryo culture stage, these poor quality eggs typically fail to make good blastocysts so IVF helps us to find the best embryos for transfer to the patient. The most important treatment for PCOS patients, in preparation for IVF, is for them to make the lifestyle changes that contribute to normalizing their hormone parameters. A good fertility doctor will outline the dietary and exercise changes that will improve pregnancy rates. There are also medications that will help normalize the metabolism so patients produce better quality eggs.
During the IVF cycle, the provider will monitor the patient closely to ensure that the patient does not get ovarian hyperstimulation syndrome and adjust the type of medication and doses during the cycle.
With lifestyle improvements and careful monitoring, IVF in PCOS patients is very successful.
The process of IVF itself does not lead to multiples. However, there are specific reasons as to why women who undergo IVF have a higher percentage of multiples. The main reason for multiples during IVF is the transfer of more than one embryo. If all the embryos implant, then multiples births will ensue. Often when women have 4 or more children during one pregnancy, this is a result of extreme circumstances like physician malpractice (there are strict guidelines stating how many embryos should be implanted), the patient was not monitored closely while on treatment, or there were too many embryos transferred. Octomom’s physician lost his California license due to the high number of embryos he transferred when clearly she did not understand the risks of transferring so many embryos.
Multiples often lead to premature births which lead to health issues for the newborns and endanger the mother. According to the March of Dimes, almost 60% of twins and 90% of triplets are born prematurely (before 37 weeks). It is highly encouraged by ASRM (American Society of Reproductive Medicine), to transfer one embryo in healthy patients under the age of 37. For patients 38 or older, multiple embryos can be transferred if PGS is not performed.
In addition, the costs and risk of birthing multiples are actually quite high compared to a singleton (or one child). A recent study stated having one child will cost about $21,000 but having twins raises the price to $105,000.
Multiples are a result of transferring multiple embryos back into the womb. If all embryos attach to the uterine lining, a woman will conceive with multiple pregnancies. 10 or more years ago, it was common to transfer multiple embryos. This was because the technology was less advanced and we had few ways of determining competency of the embryo. Typically, in older women, it was common to transfer more than one embryo because it was believed to lead to a higher chance of a successful pregnancy. However, today we have technology (growing embryos to the blastocyst stage) and tests (such as PGS and PGD and ERA (endometrial receptivity assay)) to determine which embryo is most likely to implant in the uterus. Because of these medical advances, we at Reproductive Health Center strongly encourage the transfer of one embryo at a time to assure the best chances of a healthy baby and mother.
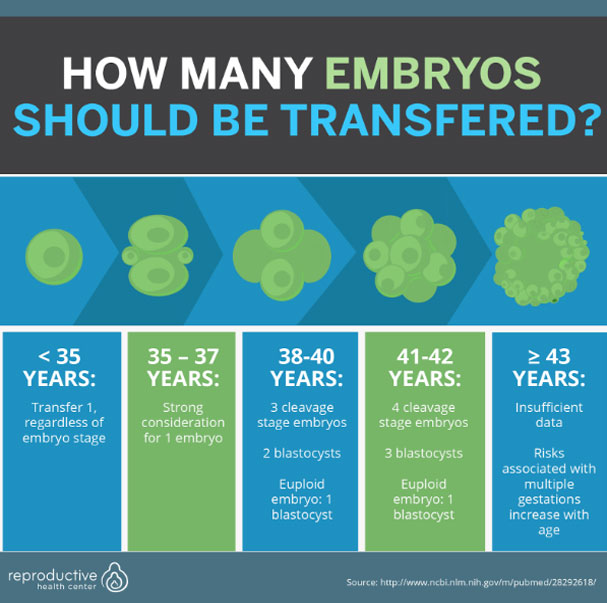
Your provider will have a very detailed discussion with you about the right number of embryos to transfer based on your specific situation.
When a patient is unable to use her own eggs to conceive, eggs from a donor become a viable option. The pregnancy rate using donor egg is much high because the donors are young women who have healthy eggs and no known fertility problems. Donors have gone through an extensive screening process before donating. Patients can choose their donor based on physical characteristics, age, education level and family history. Most clinics partner with egg banks and at RHC, we choose to partner with Fairfax Egg Bank.
You can choose to create an embryo with your partner’s sperm or utilize the sperm of a sperm donor. The donor eggs will be taken into the lab, inseminated or injected with sperm and made into embryos. The patient (recipient) will have her uterus primed for transfer by taking medications that will prepare the uterine lining for implantation. While some patients (if they are able) prefer to carry the pregnancy, it is sometimes necessary to use a gestational carrier.
The rates of success with donor eggs are higher because age and poor egg quality are the most common reasons for failed pregnancies. When using a donor, the success rate will reflect the donor’s age. So a woman who is 41 years old, using the eggs from a woman who is 22 will have similar pregnancy rates to that of a 22 year old. Although not a guarantee, many patients with their own fertility issues will carry successful pregnancies through the use of donor egg. Approximately 12 – 15% of all IVF cycles involve donor eggs and success rates are usually over 50%, with some clinics having success upwards of 70%. You can see the 2016 national average for donor eggs below.